Life insurance is about the financial protection of families over the long term. While short-term catastrophe may unexpectedly end or shorten a projected life expectancy, most are infrequent and priced into our life insurance products. But occasionally, events occur that impact most of the population; the SARS-CoV-2 epidemic has been such an occasion.
The global short-term cost of the pandemic is enormous, with projections of sixteen trillion dollars¹. While the impact for insurance claims is high, they fall within the capital reserves that our industry maintains. However, the short-term losses may only be a small portion of the future cost of SARS-CoV-2.
When cases first occurred, the clinical picture was elderly patients hospitalized with severe life-threatening respiratory lung disease. As our understanding of the underlining mechanism evolved, it soon became apparent that the infection was far more widespread than the lungs. Additional affected organs included the heart, liver, kidneys, brain, and the endothelial lining of the vascular system. It now appears that any tissue with ACE2, type 2 angiotensin receptor were targets of infection.
Survivors of symptomatic COVID-19 infection originally introduced the name “long-hauler.” It is now apparent that the term also applies to a much larger group that was asymptomatically infected. The clinical basis for long-haulers is the constellations of poorly understood symptoms that may persist for months after the resolution of the infection. Those symptoms include:
- Fatigue
- Shortness of breath or difficulty breathing
- Cough
- Joint pain
- Chest pain
- Memory, concentration, or sleep problems
- Muscle pain or headache
- Fast or pounding heartbeat
- Loss of smell or taste
- Depression or anxiety
- Fever
- Dizziness when you stand
- Worsened symptoms after physical or mental activities
Clinically, months after clearance of the virus, magnetic resonance imaging (MRI) studies demonstrate structural damage to the heart in 78/100 (78%) patients². These findings occur independently of the severity of the infection and clinical course. In addition, endomyocardial biopsy in patients with abnormal MRI documents lymphocytic inflammation in the myocardium of 60% of patients³. These findings are a significant concern in the future management and potential changes in the mortality of these patients.
Mental fog is another common complaint without a clear explanation; this includes cognitive dysfunction, including memory loss with loss of concentration, anxiety, depression, loss of taste and smell. After clearing the COVID-19 infection, the ongoing inflammatory and vascular changes that persist may provide the molecular mechanism for the neuropsychiatric symptoms. This proposal is speculation and requires research to determine its correctness.
CRL Research Summary
We examined the seroprevalence of COVID-19 in the insurance applicant population. Serum samples for 138,696 insurance applicants were analyzed for antibody to COVID-19 nucleocapsid protein (NC) with the Roche SARS-CoV-2 test. Antibody to Nucleocapsid documents infection, not vaccination. Testing was at approximately three-month intervals. We have previously published parts of this data⁴⁵.
Table 1. Seroprevalence of COVID-19 by applicant sex at four time periods.
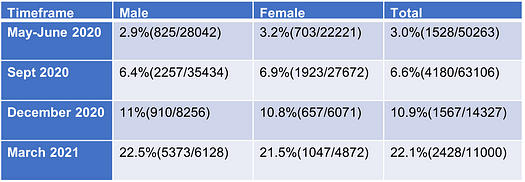
Table 2. Seroprevalence of COVID-19 by age band and test period.
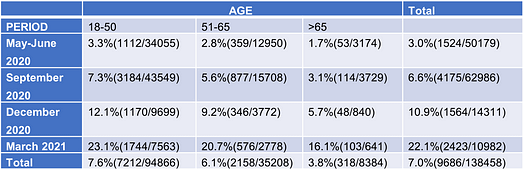
Conclusions: Currently, more than 25% of the insurance applicant population is seropositive for antibodies to COVID-19, indicating prior infection. In contrast to hospitalized patients, the highest prevalence is in the younger age group, under age 50. In addition, the long-term cardiovascular, cerebrovascular, and chronic inflammatory risk in recovered applicants is currently unknown. With this in mind, those “long-hauler” applicants present a tough underwriting challenge.
References
1. The COVID-19 Pandemic and the $16 Trillion Virus. David M. Cutler, Ph.D.; Lawrence H. Summers, Ph.D. JAMA. 2020;324(15):1495–1496. doi:10.1001/jama.2020.19759
2. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19) Valentina O. Puntmann, MD, Ph.D.; M. Ludovica Carerj, MD; Imke Wieters, MD; et al. JAMA Cardiol. 2020;5(11):1265–1273. doi:10.1001/jamacardio.2020.3557
3. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Chaolin Huang, Lixue Huang, Yeming Wang, Xia Li, Lili Ren, Xiaoying Gu, Liang Kang, Li Guo, Min Liu, Xing Zhou, Jianfeng Luo et al. Lancet 2021 Jan 16;397(10270):220–232. doi: 10.1016/S0140–6736(20)32656–8. Epub 2021 Jan 8.
4. The Silent Pandemic COVID-19 in the Asymptomatic Population. Robert L. Stout, Ph.D.; Steven J. Rigatti, MD doi: https://doi.org/10.1101/2020.12.29.20248985 January 04, 2021 DOI: 10.23880/Epidemiology International Journal-16000175
5. Seroprevalence of SARS-CoV-2 Antibodies in the US Adult Asymptomatic Population; Robert L. Stout Ph.D; Steven J. Rigatti, MD https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2777502 Mar 16, 2021
About the Author
Dr. Robert Stout serves as Chief Scientific Officer and Laboratory Director for CRL’s General Laboratory. He provides scientific direction and research leadership for all of CRL with particular focus on research for CRL’s Insurer Services business. Dr. Stout, who has been with CRL since 1983, holds more than ten U.S. Patents in science, including one for immunoassay method and apparatus development (U.S. Patent #4,414,324) and one for methods of determining chronic Hepatitis C infection (U.S. Patent #10,051,253). He is the author of numerous research and review articles and is a regular presenter at scientific meetings and conferences. Dr. Stout holds a B.S. in Biochemistry from California State University and a Ph.D. in Biological Chemistry from U.C.L.A. School of Medicine.
COVID-19 & Children: Can We Trust Published Data on Masks?
Dr. Michael Fulks, consulting MD, comments on June data about COVID-19 mask-wearing for children. This timely article – and the associated comments and subsequent redaction – is of particular interest to the CRL team, with school-aged children approaching the start of another school year. Read below to get the facts from Dr. Fulks.
A research letter in the June JAMA Pediatrics issue, authored by Harald Walach, assessed the CO2 content of inhaled air in children using and not using masks. It was of great interest to me given the likelihood that school-aged children will return to in-school teaching this fall and may need to be wearing masks indoors. I had previously looked for data on this subject and been disappointed by the limited amount and quality.
This study looked at 45 children, average age 11, each without a mask and while wearing two different masks measuring CO2 levels through a tube taped on the face near the nose. The conclusion of the article that masks increased CO2 levels and may lead to “hypercapnia” and should not be worn by children was unsettling. However, I found the study protocol and results showing increased CO2 levels under the mask during inspiration difficult to interpret and some of the wording and references suggested potential bias. On the other hand, this paper was published in a peer-reviewed JAMA journal, with no definitive data to refute the data or conclusion out of hand.
Just two weeks later, the piece was formally retracted by JAMA Pediatrics. Comments to the editor that led to the withdrawal noted the author’s psychologist background with no expertise on the issue, an anti-COVID restriction group as the funding organization, inexplicable findings based on the CO2 measuring device, and inconclusive findings about the max level of CO2.
Doing good research is hard and reviewing it is often even harder; I have done both and had my share of failures. But publishing this biased inaccurate report on the highly politicized and emotional question of mask wearing by children is a clear disservice to the community. To their credit, the editors reacted quickly to the resulting comments they received. I do wish for more accessible published data on the subject, but available research and considerable real-life experience indicate masks do not harm children while reducing COVID-19 transmission.
If you have questions about COVID-19 data, our doctors are here to help demystify and explore the findings. Feel free to email us at ILSblog@crlcorp.com with concerns or comments.